Gautam Dongre’s two children in India and Pascazia Mazeze’s son in Tanzania live with an inherited blood disorder that turns blood cells into instruments of pain.
New gene therapies promise a cure for sickle cell disease, and Dongre says he’s “praying the treatment should come to us.”
But experts say the one-time treatment is out of reach in India and Africa — places where the disease is most common. Vast inequities cut much of the world off from gene therapy in general.
While access to all sorts of medicine is limited in developing countries, the problem is especially acute with these therapies, some of the most expensive treatments in the world.
Beyond their sky-high prices, these therapies are extremely complex to give patients because they require long hospitalizations, sophisticated medical equipment and specially trained doctors. So far, the two gene therapies for sickle cell have only been approved in wealthier countries: both in the U.S., and one in Britain and Bahrain as well.
“The vast, vast majority of patients live in an area where they have no access to this kind of therapy,” said Dr. Benjamin Watkins, who treats sickle cell at Children's Hospital New Orleans. “We as medical professionals, and as a society, have to think about that.”
Access to gene therapies was a major focus of this year’s international summit on human genome editing in London. A subsequent editorial in the journal Nature said high prices leave low- and middle-income countries “entirely in the lurch” and could stymie progress across the field.
Some scientists worry that new cures won’t reach their potential, future treatments may never be invented and the prospect of wiping out diseases like sickle cell will remain a distant dream.
STRUGGLING FOR BASIC TREATMENT
For gene therapy to even be an option, people in developing nations must stay alive long enough to get it. There, sickle cell disease is more likely to disable or kill than in wealthy regions. Late diagnosis is common and basic care can be hard to come by.
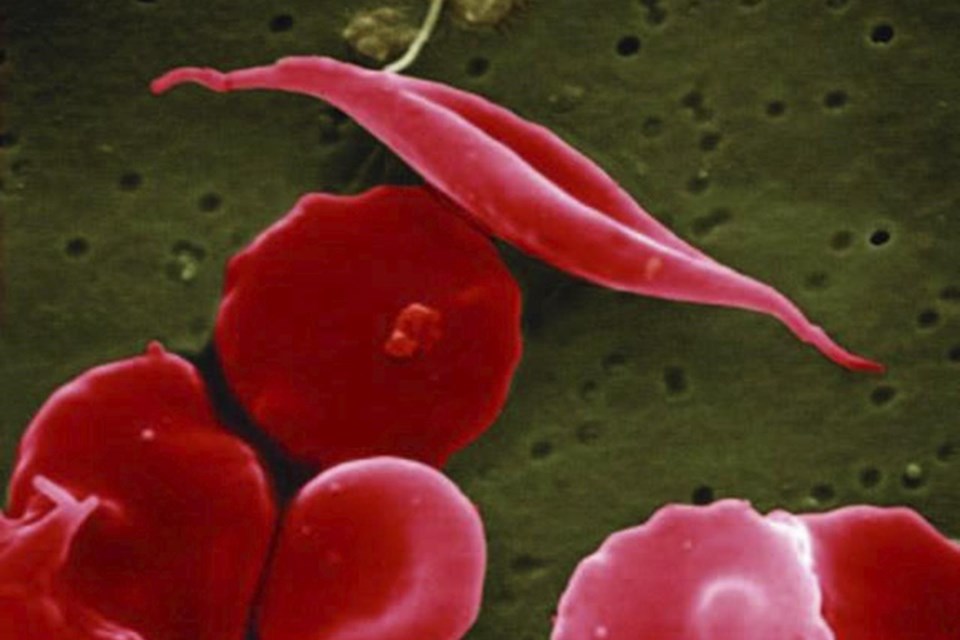
Sickle cell disease affects hemoglobin, the protein in red blood cells that carries oxygen. A genetic mutation causes the cells to become crescent-shaped, which can block blood flow and cause problems such as excruciating pain and organ damage.
Global estimates of how many people have the disease vary, but some researchers put the number between 6 million and 8 million — with more than 1 million in India and more than 5 million in sub-Saharan Africa.
Dongre, who lives in Nagpur in central India, has seen the struggles in his own family and among people he’s met as a leader of India's National Alliance of Sickle Cell Organizations.
He recalled how his newborn son Girish cried constantly from stomach and leg pain. Doctors didn’t diagnose him with sickle cell for 2 1/2 years. When their daughter Sumedha was born, he and his wife had her tested immediately and learned she had the disease too.
Available treatments can reduce the bouts of pain known as “crises.” Dongre’s children, now 19 and 13, take hydroxyurea, a decades-old chemo drug that helps prevent the formation of sickle-shaped red blood cells and control the disease.
Other patients in rural areas are dying at very young ages without getting the right treatments, Dongre said.
The situation is much the same in East Africa's Tanzania.
Mazeze scrambled for information after her son, Ian Harely, was diagnosed.
“I Googled and Googled and I couldn’t sleep,” said Mazeze, executive director of the Tanzania Sickle Cell Warriors Organization. “After that, I was praying. It was God and Google.”
Her son is now 10 and takes hydroxyurea and folic acid for anemia. They’ve helped, but haven’t eliminated pain episodes.
Still, Mazeze counts herself lucky she can afford treatment at all. She said some in Tanzania can't even pay for folic acid, which costs less than a dollar.
’SIGNIFICANT CHALLENGES’
Such stark realities make the cost of gene therapies an insurmountable obstacle, experts say. The price tags for the two sickle cell therapies in the U.S. are $3.1 million and $2.2 million although costs can vary by country.
The process of giving the therapies is just as big a hurdle.
Patients must go to the hospital, where stem cells are removed from their blood. One treatment, made by Vertex Pharmaceuticals and CRISPR Therapeutics, involves quickly sending the cells to a lab and using a gene-editing tool called CRISPR to knock out a gene.
The other therapy, made by Bluebird Bio, doesn’t use CRISPR but involves the same process for patients. They must undergo chemotherapy before they get back their altered cells, and spend weeks in the hospital. The process can stretch on for months.
“There’s great unmet need, but there are also significant challenges,” said Dr. David Altshuler, chief scientific officer at Vertex.
Scientists are working to make easier-to-administer versions of the new therapies. Altshuler's team is trying to develop a pill that wouldn’t edit genes but would have the same goal: helping the body produce a fetal form of hemoglobin since the adult form is defective in people with sickle cell.
But experts say simpler cures will likely still be unaffordable to many, so foundations and governments will be instrumental in getting them to patients.
If the gene therapy eventually makes it to India, Dongre would like his children to be among the first to get it. Mazeze said she may wait to see how other patients fare but will consider it for her son too.
Both agreed it should be an option in all countries — rich or poor.
“We all are part of one single planet,” Dongre said.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
Laura Ungar, The Associated Press